
Not exactly the words you want to hear from your doctor. Getting white-glove treatment at a hospital is usually not a good sign. Those words triggered an avalanche of thoughts and fears, but the journey was just beginning. And just like that, everything changed.
But to understand how I got to this moment, I need to rewind a week... I was getting ready to fly to Washington D.C. for a work trip. We were seeing a resurgence of COVID at this time with the new strain of Omicron to add on top of the Delta variant that was still prevalent. I needed to self-test to get on the plane (it was a chartered flight). I tested a few days before and it was negative. On the day of the flight, I was feeling run-down. Tired and a bit lethargic. I had a sneaking suspicion that COVID might be incubating inside of me, so I tested again. Still negative.
I made the trip and concluded I have the pandemic flu. I was mentally tired, and it was manifesting into my physical energy. We had our first family winter vacation scheduled in just over a month. I was hoping it would be just what the doctor ordered.
Instead, the doctor ordered a very different cocktail, far from the Pina Colada I had in mind. Little did I know, this assumption was the first of many misdiagnoses I would make as my condition worsened.
What I initially dismissed as mental fatigue soon revealed itself as something more sinister. Over the next few days, new symptoms began emerging that I couldn't explain away. While flossing, my gums began to bleed. Then I was ambushed by nosebleeds, sneaking up on me when I least expected it. Thank goodness for masking, or I would have recreated a scene straight out of The Shining at work.

I made it through the week at work and into the weekend. I was in an empty house since my oldest son was at college, and my wife (Kristen) and youngest son were at a dance convention. I was still lethargic and still dealing with bleeding gums. I did some armchair doctoring and determined I was anemic. I had a nasty cold for about a month before this that I suspected came from my college son. It seemed likely that anemia was just the hangover from that cold. A virus that had mutated through keggers and questionable choices, passing through hundreds of college kids. I did a some research and scoffed at one of the top search results of Leukemia. People assume the worst of a rare disease when it ends up being a common cold. The news was filled every day with overcrowded hospitals and the last thing they needed was somebody where the prescription was sleep and chicken noodle soup.
My at-home remedy was iron supplements for self-diagnosed anemia and plenty of rest. I took iron pills and promptly fell into a deep sleep. Normally my internal alarm clock prevents me from sleeping in, no matter how late I stay up, but today it stayed silent. I eventually got up and tried to be productive by walking our dog, but then ended back on the couch for another nap.
Fast forward to Sunday night. My wife comes home and convinces me to go to Urgent Care. It didn't take much to convince me because in the back of my mind, I knew something else was going on. The nurse at Urgent Care calls me in, asks me some questions, and decides to draw blood. Her leading root cause was gingivitis and the lurking after-effects of the Zombie-Apocalypse starter kit cold I was recovering from. At the end, she tells me "Results from the labs will be in on probably Tuesday. Go see your doctor tomorrow." Ok, that growing weight in the back of my mind just had another brick thrown on it.
I didn't have a family doctor. If I needed anything, I went to Urgent Care. Managing my health proactively just didn't happen for various reasons. My wife made me an appointment on Monday morning where the rest of the family goes and I have my first official family practitioner in over 15 years. This visit would put us all in the deep end.
She took my vitals. Then she poked, prodded, and landed on two possible scenarios. I could have some strange immune-triggered response to the Virus-Gone-Wild cold I had or maybe a blood disease. This wasn't the end of the terrible "A" or "B" scenarios. We started rooting for the Virus-Gone-Wild immune issue while we wait to get the lab results back.
Tuesday rolls around and I still feel terrible. I have a pain in my thigh and in my upper shoulder blade from where our dog bolted after a squirrel while walking her over the weekend. I had a constant taste of blood in my mouth from my gums that would bleed during brushing my teeth and linger on throughout the day. No problem. I had one important meeting to attend, and after that, I planned to be out the rest of the week. I knew I wasn't right and this wasn't going to be a simple case of treating it with iron and chicken noodle soup. I had already exhausted that remedy anyway.
After my meeting wrapped up, I headed upstairs to lie down. My wife soon joined me. Her phone rang, and I heard those words that sealed the weight of the moment..."You need to get to the ER. We have a Hematologist waiting for you."
We packed a day bag, but I paused and told my wife I needed a moment. I sat on the edge of the bed as the weight I was carrying came crashing down. I may not see my home again. Ever. I packed the thought into the back of my mind and gathered myself. We quietly made our way out of the house and to the hospital. I had to keep it together, for Kristen, for my boys, and for myself.
Emergency rooms were not a place to hang out. They were filled with COVID cases and they arranged expedited service for me. I didn't realize yet how familiar these hallways would become, or how often my life would hang in the balance here.
They had to get a room ready for us, so they recommended we wait outside. It was early November and freezing, but it was a better alternative than sitting next to the infected monkey from Outbreak in the waiting room.
During the wait, they gave us heated blankets as we sat on a bench outside the entrance. We got to see a patient "check" himself out, IV still attached. They came out and got him, explaining that you can't just get up and leave. Turned out he just really wanted a cigarette. I found this both funny, but also a bit terrifying. I was already getting stir-crazy at the hospital and we weren't even 20 minutes in. I was dreading the rest of the day. The hurry-up-and-wait. The inevitable two-hour delay just to get checked out and released to go home. Ah, how naïve I was in the moment.
Kristen and I get brought back to a room in the ER and they ask me to change into a gown. Up until this point in my life, I had never personally been in a hospital outside of seeing relatives. My first moment of panic was the gown. I whispered to Kristen, "do I get all the way naked under this thing?". She gave me a laugh, but she wasn't quite sure. I was getting prepared to go down to my birthday suit but decided to ask. Ok, just my shirt off. I'm a modest person and was about 30 seconds from baring it for all to see. This was also the point where my modesty was going to have a rapid decline over the course of the next month.
They proceeded to take 6 vials of blood. So much blood. I was sitting in awe that I could give that much that quickly and not be impaired. The body is amazing with its intricacies and complexities. My curiosities around this were about to get a nice scratching through this experience.
After sitting for about an hour, I see a doctor who says they are going to admit me as soon as a room was available. Throughout this, I had a coping mechanism. It was dark, morbid humor. I was making jokes to Kristen that tried to make fun of the situation by making fun of the worst outcomes. I thought it was hilarious at the time. Kristen did not. I would soon come to appreciate that it was selfish behavior that manifested itself in other areas of my life and it would soon be eradicated. Soon, but not that day. The gravity well was pulling us in further, but we were still on the edge of the Event Horizon.
My blood results showed I had low platelets. I was at 16 where 150 was considered the bottom-end of normal. Everything was low. So low that I was at high-risk for infection, but the more concerning part was clotting. If I were to fall or injure myself, there was a high likelihood of hemorrhaging. I was wheeled up to my room, put in my bed, and told to keep movements minimal.
This is the date I was admitted into the hospital. This was when I was told I have a blood cancer.
Remember the first "A" or "B" scenario where it was Crazy Virus Immune Response vs. blood disease? Well, the next one I got was you have leukemia, but we need additional testing to verify the type. You either have AML or APL. AML is one of the worst types of Leukemia and is more common. APL is very rare and the one with the highest cure rate. Alright, I vote for sucking less. Come on APL!
They decided to immediately start treating me for APL, since the lab results would take two days and the treatment for APL couldn't hurt. They also had a pretty sure idea it was APL, but they can't officially diagnose without the PML-RARA gene test. This test looks to see if chromosome 15 and 17 did a switcheroo - the tell-tale indicator of APL.
The treatment for APL turned out to be just as unusual as the cancer itself.
It involved a combination of Arsenic (ATO) and megadoses of a vitamin A derivative (ATRA). The fun part on ATRA is that a topical version of it is used for acne. You might know of it as Retin-A. The cure for what ails ya? A little bit of intravenous rat poison with a cocktail of acne medication.
Day 2 and I started feeling some side-effects. Blurred vision, a little bit of a headache. My arm has been repeatedly poked, with each one leaving a bruise. No sweat. I got this. When can I go home?

End of Day 2 and it's confirmed. I have acute promyelocytic leukemia. To put it simply, your bone marrow is a factory for blood cells. Mine developed a defect in the system and started switching up chromosomes 15 and 17. This results in useless blood cells, which crowd out the good blood cells (white, red, platelets). Yeah science!
The side effects I was experiencing during the day were nothing compared to what awaited me that night. Hospital nights (and coincidnently shift changes), I would learn, are when your body's distress signals become impossible to ignore. They don't tell you this about hospitals, but you don't go there to recover. You go there to get treated. It's about as effective of a place for recuperation as 1999 Woodstock. You are getting checked every 3 hours, beeping machines throughout the night, and patients verbally expressing their physical and mental suffering in new and interesting ways.
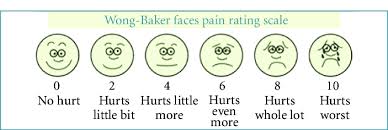
My body is already aching. Those pains in my thigh and shoulder are persistent and nagging. Laying in a bed only made them worse. Having a body that could not heal amplified and prolonged the pain even more. On the 1 to 10 pain scale with the faces they use, I was a 3.
Approaching 1am, my thigh bones were throbbing. I start rubbing them, but it just keeps building.
I am a painfully prideful and independent person. I won't ask for help. You'll find me wandering the aisles at Home Depot and pulling up their map on my phone before I would ask one of the employees where I can find door hinges.
This pride kept me from asking for help from nurses earlier. I have a higher threshold for pain, so I thought I just needed to ride it out.
I remember seeing that pain scale at a hospital and thought a 10 on the scale would have to be William Wallace in Braveheart where they are torturing him by removing his insides while he was strapped down. No way would I ever be at a 10.

By 5am, I'm sweating and tearing up from the pain. My bones literally felt like they were exploding and shredding. I tell the nurse I'm a 9/10 and she is working on getting pain medicine cleared from pharmacy. I didn't firmly commit to the 10, but I couldn't imagine worse pain.
I get a shot of Dilaudid, a heavy hitting opioid. Within 10 minutes, the sheer relief of the pain subsiding almost brings me to tears of relief. There was also an anti-inflammatory that was used sparingly at this time, but it was a miracle drug. I can't find a record of what it was, even though I told Kristen I was going to be buying stock in it. I found this drug more effective than Dilaudid, and as luck would have it, I had to limit the use since my liver was already getting hammered.
My new opioid friend would be called upon several times over the next few weeks, and I needed it. On this day, the hospital also put a new "no visitor" policy in place because of the rise of COVID. While my stay wasn't solitary confinement, it was close. I had doctors, nurses, my phone, and a TV.
The next day we continued treatments as normal. This was the last glimpse of normal I would have for quite some time.
While APL has the highest cure rate of all types of leukemia, that doesn't mean it's benign. The high cure rate is based on patients that make it through their first month. The first month is fraught with complications from the side-effects of the cancer. That's why they essentially keep you nearly bed-ridden since the number one cause of fatalities is from hemorrhaging.
In my case, I had stacking symptoms that put the probability of my survival in the low teens at one point.
By Day 4, I was swelling and showing symptoms of differentiation syndrome, a side effect of the treatment that forces immature blood cells to mature (or "differentiate") rapidly. Unfortunately, in about 20% of patients, this process can happen too quickly and intensely. Once again, I hit the lottery. In just 4 days, I had gained 20 pounds. The swelling was extreme — my feet looked like they were about to burst. And it wasn't just my feet; the swelling also reached my heart.
I started feeling pain in my chest. Having learned my lesson, I knew to ask for help. I explained to the nurse, but I still discounted it. I thought it might be heartburn. I had heard people mistaking it for heart attacks, and I didn't want to be a bother again. The nurse said it might be, so she gave me some Tums. Hmm. Not working. If this is heartburn, I felt terrible for people who got it. It felt like someone was tightening a vice around my heart. Each breath was a painful reminder that something was terribly wrong.
Well, it continued. It continued to where I could only take rapid short breaths. It continued to where it was crushing pain. It continued until I was surrounded by doctors and nurses with the "crash cart" ready to jolt my heart.
They couldn't find anything that was causing it. They did EKGs and didn't see anything. My opioid friend lent me a hand and got me back from a 9/10 on the pain scale (still not calling it a 10) down to a 4. I can deal with a 4.
The silver lining is that because my condition was critical, Kristen could come in to see me. She quickly came in and I filled her in on my eventful morning. A morning where the story hadn't been fully told yet.
She helped me get to the bathroom. As I was sitting, I became extremely lightheaded, and I had a very hard time breathing. I sat on the edge of my bed and hit my call light. I crumbled back down on the bed and round 2 started.
One of the most difficult parts of my leukemia happened in this moment. I laid in the bed, surrounded by staff, to see Kristen standing in the corner to stay out the way. In my suffering of that moment, nothing hurt more than knowing she was in the room and watching me potentially die in front of her. She was calm and didn't let her panic show. Her strength was amazing.
In this moment, I also found my mental breaking point on toughness. I declared a 10 on the pain scale. I was in agony and sweating so profusely that the stickers on my chest to connect wires kept sliding off. Even though I was already doped up, I felt like the Incredible Hulk burning through a tranquilizer. It just wasn't working.
The tests were still not showing anything on my heart. I couldn't breathe. It was so painful with each breath it was essentially hyperventilating. One of the nurses tried to use the data (or lack thereof) and said, "You can breathe. You are talking". Ok, smart ass. It really, really hurts to breathe and I don't like to choose between air and pain.
Now the root cause started to show up in the scans. Fluid was rapidly building up around my heart. It was crushing my heart and inhaling was adding additional pressure. I was given the miracle anti-inflammatory and it was amazing how effectively it worked.
They needed to do an emergency surgery to drain the fluid. They found a doctor who could do it and didn't even have time to get the CYA paperwork signed. They asked me for verbal consent, and I gave it to them.
There is a sac that surrounds your heart called the pericardium. Between the sac and the heart is a small amount of fluid as a lubricant. There is maybe 50cc's present under normal conditions. In my condition, they pierced the sac and drained 500cc's. That's half a liter of soda right there.
These side-effects led to them stopping treatment for leukemia. This was crushing news, because I still had hopes of getting back home in a "few days". My own assessment. Not the doctors.

When they drained the fluid, they found it was also infected. How? They weren't sure. I didn't have infection in my blood, so it was a mystery around how it was infected around my heart. It remains a mystery even to today, although I do have my own speculation. I had a PICC line put in on Day 3. This is essentially fixed access on the vein inside the bicep of my arm. It gives easy access without needing to poke me each time. It runs a line that hangs right above your heart and dumps medicine right into your heart. No poking and efficient distribution of medicine. Win-win. Except if nurses aren't exceptionally clean. This happens a lot since the quality of nurses varies a lot.
I believe the infection came from getting the PICC line or perhaps one of the many times I was poked. It led to the infection. This also led to now having 3 specialist doctors - oncology (the leukemia), cardiology (the heart), and infectious disease (the infection in the heart fluid).
The fluid kept building up again which prompted the need for my second heart surgery. The first one was minor where they poked the sac and drained the fluid. This one needed to be a bit more. A pericardial window is where they create an opening in the sac - the "window". The doctor that could perform this was at a different location. They found an opening and arranged the transfer to a nearby hospital.
I was over a week in the hospital. When I was transferred, it was the first time I had breathed fresh air since being admitted. It was a brief window of 30 seconds from the door to the ambulance, but it was treasured.
The next surgery seemed to go smooth. However, I woke up and felt like Neo when he was in his pod as a hardwired battery in the Matrix. I had a quarter-inch drain tube running below my sternum up to my heart. I had a catheter. No big deal, right? Not in the grand scheme of things except I didn't know I would have one. I woke up and surprise!

Not really. Since I was on extremely high doses of steroids and low platelets, I wasn't healing. I had soreness when swallowing for two months after being intubated. The 2-inch opening on my chest from surgery didn't heal for several months either. Even then, it didn't close. What normally would be a 2" x ¼" scar is a 2" x 1" scar that just filled in over time. Not gonna lie. It was gross.
I'm now over 2 weeks in the hospital and no end in sight. I am fighting the fluid buildup, fighting the infection, but not fighting the cancer. The main reason I'm in the hospital wasn't even the main battle I was fighting anymore. I did restart the ATRA and this ended up being key.
I'm mentally and physically exhausted. In no other point in my life have I shed so much blood, sweat, and tears.
One of the bigger milestone victories for me was getting untethered. When the catheter was pulled out, it reminded me of a magician pulling the never-ending handkerchief from their hand. When the heart drain came out, it was an odd feeling. I no longer had that feeling of a foreign object in my body. I now had the luxury of turning on my side. I now had the horror in my mind of a gaping hole from where the tube was in my body leading to my heart. I hadn't thought a lot of what happens in the space between the organs in the body until this moment. Also, the fact that a hole that big will just shut the door on the way out is amazing.
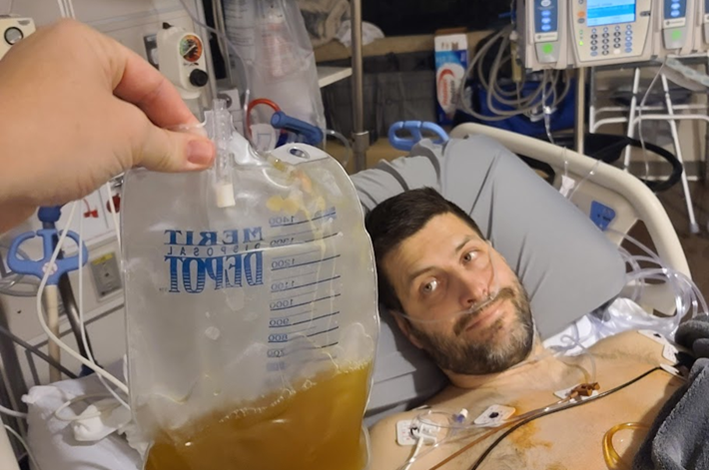
I had over 10 different blood transfusions. These were necessary to give my platelets a boost to prevent hemorrhaging and to even have surgery as an option. If it weren't for blood donors, there is a possibility that I wouldn't have survived this first month. In my endless curiosity, I was always surprised that a bag of platelets essentially looked like turkey gravy. I have many things to be thankful for on Thanksgiving, including those wonderful bags of gravy that kept me going.
This was not the kind of attention I wanted. I was a person, not a puzzle to be solved.
Being hit by three different afflictions at once was complicated. My oncologist displayed what I think is a rarer trait for doctor. She was humbled. She knew that because this was rare, she didn't have the experience and intuition to guide it. She was connected with a very well known oncologist and he was consulting with her throughout. She was also a bulldog in working to get me transferred to him. She worked at this and was very open about it. He belonged to another hospital in a different city. They were already over capacity due to COVID and were not accepting any new patients.
Infectious Disease was good throughout. They knew we had an unsolved mystery, but what was needed was to get the infection cleared up. They worked diligently on this, and my case was a bit less interesting to them.
Then there was Cardiology. There was a doctor who really wanted to help me. To the point to where I could tell it was less about helping me and more about the ability to solve a hard problem. He told me he could really help. Most of his patients were on a fixed path; they'd either make it or they wouldn't. But with me, he saw a chance to change the outcome. Because of this, he didn't want me to transfer. While I believe he had the best intentions, I didn't feel like I was at the center of it. I certainly wasn't going to advocate to not transfer to a renowned doctor for the main affliction at hand.
A simple leaf reminded me of the life I was fighting to return to. It was a turning point, where survival became about more than just making it through the day.
Thirty days in and there was a simple pleasure in my life that was given back to me for a moment. My daytime nurse during this time was amazing. She was skilled in both caregiving and empathy. My focus had been on rebuilding my strength. I've lost 40 pounds and can't walk unassisted. I've started building up my stamina by doing a lap in the hall with a walker.
She came to me one day and told me to get dressed. I put on my robe, thinking we are going for a lap. She shows up with a wheelchair and tells me to get in and to bring my phone. She takes me to the elevator and took me outside. This was during a warm spell where we just had a massive windstorm that took out power in a lot of places. She parked me next to a bench and left me. I was able to feel the sun. Feel the wind. And then it hit me - a leaf. It hit me in the face, and I melted into uncontrollable sobbing. I didn't feel like a test subject for that moment. I felt like a human being again. I video-called Kristen, but I couldn't really speak because of the emotions. We shared the moment, and it was the first time I felt like I was doing more than just surviving. I was living.
After over a month of being admitted I was given my transfer to the University of Michigan hospital as a patient of Dr. Bixby. I once again packed up my belongings and was wheeled off for an ambulance ride as an official transfer to a new hospital 30 minutes away.
I arrived and there was a noticeable difference. There was confidence and consideration. It's not that the other doctors weren't good, but it stood out that there was experience with my rare condition. We weren't starting the ATO, but I was still taking the ATRA. They were developing the plans, but the future still wasn't clear. My goal to get home by Christmas was looking less likely each day, but I felt like I was on a clearer path forward.
The primary focus was still to get my heart under control. My resting heart rate was still high, and I was still having occasional feelings of constrictions. Before we could really attack the cancer, we had to stabilize my heart. Sometimes you have to put out the fire in the kitchen, before you fix the gas leak in the basement.
I took advantage of the food while in the hospital. While it wasn't exactly gourmet, there was a decent selection and I was intent on putting some weight back on. I had even gotten into the habit of ordering hospital fish when it was on the menu on Friday.
A clear bonus and factor in my recovery (especially mental) was that the new hospital allowed visitors. This let me consistently see Kristen again. No more playing Scrabble on our phones together. We could be together.
This also let her be my food smuggler. It was allowed, but it sounds better to picture her smuggling sub sandwiches inside her jacket.
I had spent a month watching nothing but Food Network. I was desperate for some Iron Chef level food. My first experience was a world-renowned delicatessen right inside the same city as our hospital. This ended up being a stress on my heart. While I wasn't overly excited, my heart disagreed. As soon as Kristen pulled out the food, my heart rate spiked to 175bpm and triggered alarms. It took some Zen-like meditating to pull it back down and eventually have the chance to eat it.
My last mental breaking point came around day 38. My heart was at a stable enough point that we could consider restarting the treatment of the cancer. This meant I was being transferred to the Oncology floor and into a new room. This was also the first time I shared a room during the entire experience since I was immunocompromised. Since I wasn't in active chemo treatments and space was tight, I could have the risk of a roommate.
This came with a new host of surprises. The first was that they had to keep me attached to my PICC line all the time. This triggered a deep response in me. It was traumatic to be tied down with tubes and I associated this with decaying. I asked them to let me sign-off on the risk. Nope. I asked for any type of creative solution. We finally landed on a compromise. I had a new "temp" line added on my left wrist. It was uncomfortable, but their policy allowed this to be disconnected after getting an IV.
The next new change was testing for MRSA. Ok, that makes sense. Until they told me how they tested. It involved the only place on my body that hadn't been poked and prodded during this stay. The last inch that was still private and personal. On the first day and every Wednesday, they had to swab where the sun doesn't shine. I stood up, dropped my drawers, and exhaled my last breath of dignity.
At this point, I spent most of my time trying to rehabilitate. I was walking laps in the hallway that equaled 2 miles every day. I was getting stronger, but I was still a shell of myself from over a month ago. Getting out of bed was a chore and walking a straight line took effort by itself. However, this was the first time where I felt like there were things I could control and do to get better. I was embracing it.
I had my second bone marrow biopsy on December 19th. My blood levels were much better, but not normal. We were hopeful the results were going to be good on the biopsy, but we had our expectations that I would not be home until early January.
It took 2 days to get the results back. In my normal morning sync with the doctors, they came in with the news. I was officially in remission, and we could start talking about going home.
Now I blame the very strong doses of steroids on my trigger emotions during the stay. During my mental breaks, I would sob. I would sob to where I couldn't communicate. It wasn't because I was sad, I just didn't seem to have control of it. I would have been able to carry on logical and rational conversations via text messages, just don't ask me to speak. However, the flood of emotions in hearing that I would be home in a few days and in time for Christmas with my family would be enough to break down Ben Stein into uncontrollable sobbing.
After 42 days in the hospital, I took my first steps out of it on my own. Walking out wasn't leaving illness behind. I would have 8 more months of chemotherapy and treatments. Walking out was stepping forward with a clearer view of what truly mattered: presence, gratitude, and to never take tomorrow for granted.
I guess Douglas Adams had these two things right in Hitchhiker's Guide to the Galaxy: the answer to the universe is 42 and "so long and thanks for all the fish" (Fridays).
The words from Kristen when we received the call from my final bone marrow biopsy stay with me to this day. It came back that the treatments had worked, and I would be done with treatments in a month. She hugged me, cried, and in between sobs said "you are so strong". One of the most powerful and sentimental moments in my life.
This wasn't the end of the story, simply a chapter I felt worth telling. Why? I originally wrote this while in the midst of chemo, the rat poison infusions inspiring my inner muse. I started writing this with hopes that it would be therapeutic. As I approach my 3 year milestone of completing treatments with clear bloodwork, my hopes are now that this helps somebody else in their own journey.
When you are in the middle of a battle, you have to put your head down and persevere. If you are reading this from a hospital bed, infusion center, or watching a loved one fight their own battle - know this. You too are stronger than you think when you take it one day (and one bag of arsenic) at a time.